Achilles tendon pathology
Regardless of whether you have experienced a trauma, or an overload through excessive exercise, pain can also arise spontaneously in or around the Achilles tendon. Different syndromes exist and can occur independently, or combined.
1. Focal nodular tendinopathy
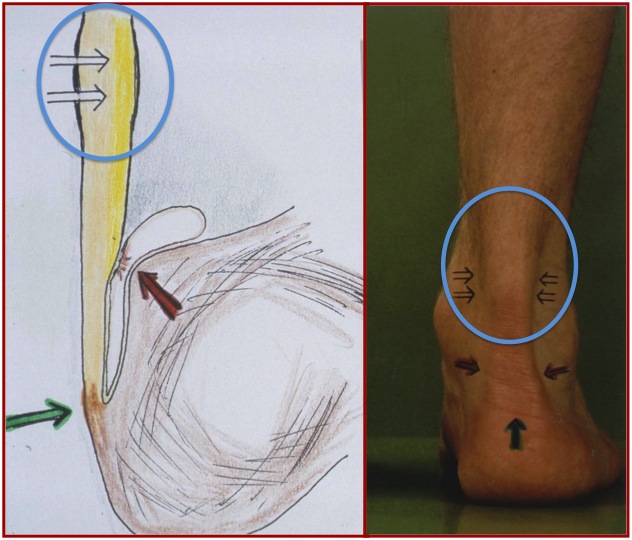
Definition
If you have pain at about 2 to 5 cm from the attachment of the Achilles tendon on the heel bone and a thickening can be felt mainly on the medial side of the tendon, it is possible that you suffer from focal nodular tendinopathy.
Causes
The real cause is not yet known, but it is believed that a small tendon, leaning against the Achilles tendon, has adhered to it, causing an inflammation and a thickening in that place.
Treatment
First and foremost one has to follow physiotherapy and wear a special ankle brace. In most cases this will suffice. However, if the pain persists, surgery may be planned in order to eliminate the adhesion and reduce inflammation. This happens in day hospital. Normally, you can immediately lean on the ankle after the operation, provided that you use crutches.
2. Non-insertional tendinopathy
Definition
This is defined as pain in the Achilles tendon itself, except at the height of the attachment to the heel bone.
Causes
Again, the real cause is unknown, but it is believed that it is a combination of reduced blood flow to the tendon, abnormal healing symptoms after a minor trauma, old age phenomena,…
Treatment
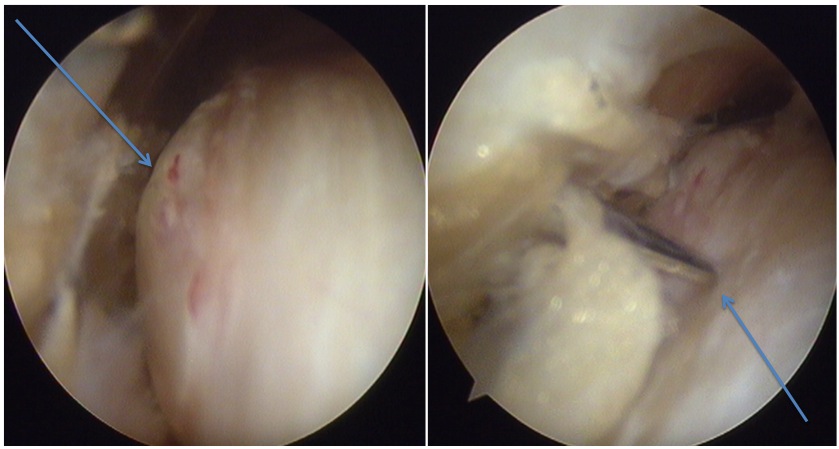
In most patients, physiotherapy leads to a reduction in symptoms and a return to the same level in sport. Alternatives are injecting concentrated platelets and/or performing a peignage. (These are small incisions in various parts of the diseased portion of the tendon, with the aim of causing bleeding, and thus to bring healing.)
3. Insertional tendinopathy
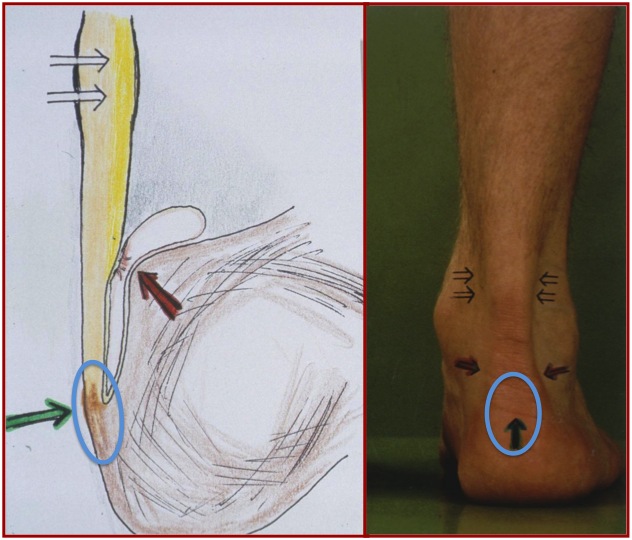
Definition
In this case, the pain is mainly localized near the attachment of the tendon on the heel bone.
Causes
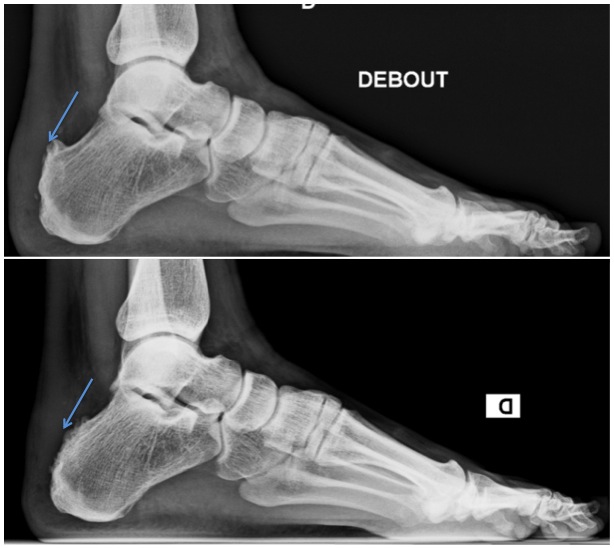
Initially, nothing can be seen on normal radiographs, but after a while certain parts of the tendon-bone transition start to calcify. This makes this part relatively stiffer than the rest of the bony attachment, which ultimately leads to inflammation.
Treatment
Treatment consists of a raising of the heel, which reduces the stress on the tendon attachment. The injection of cortisone or one of its derivatives may weaken the area and sometimes cause a rupture.
If the raising of the heel and physiotherapy don’t improve the situation, one should consider a scan to clearly identify where calcifications are localized near the attachment. Since the calcifications are present in the tendon itself, they can be removed only with open surgery. Depending on its size, one must sometimes re-attach the tendon to the bone with a bone anchor, whether or not reinforced by the transplantation of the flexor tendon of the big toe.
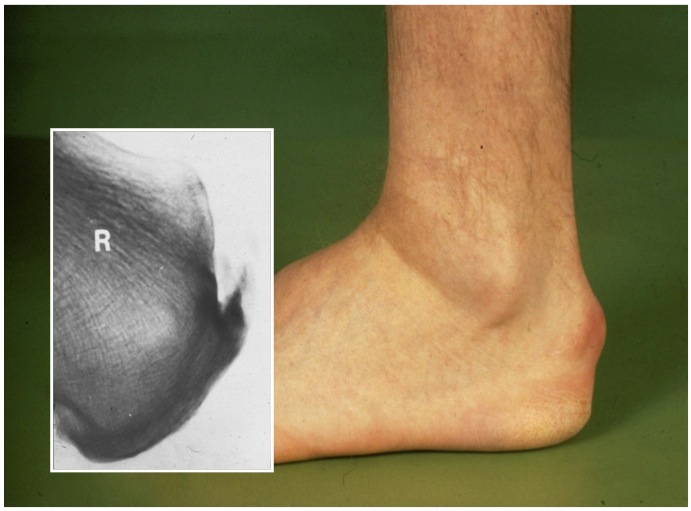
Definition
This is the situation where the bursa between the heel bone and the Achilles tendon is inflamed.
Causes
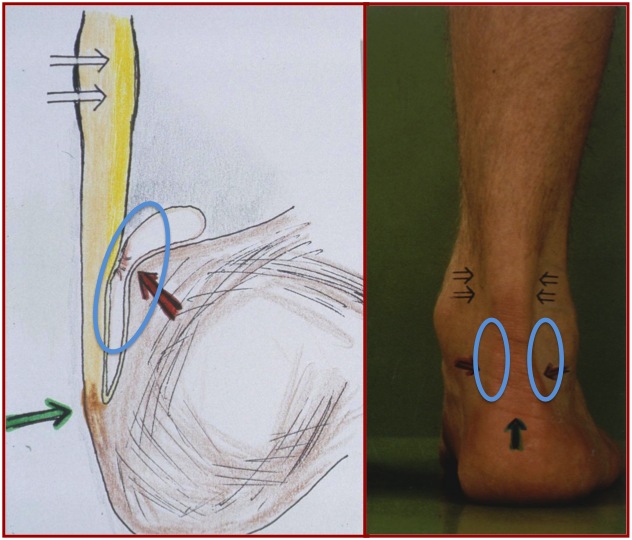
This area, which is normally very thin and almost virtual, gets swollen and inflamed because of increased friction.
Symptoms
The pain can be found just above the place where the tendon inserts into the bone and slightly to the sides.
Treatment
A raising of the heel allows the tendon to be somewhat removed from the bone and thus to reduce the friction between them. The combination with physiotherapy heals patients in most cases from “Haglund disease”.
Occasionally, surgery is considered, always with the aim of ensuring that no conflict occurs between the tendons itself and the bone:
- Our preference is to remove the excessive bone growth through arthroscopy, as the rehabilitation after surgery clearly goes faster.
- The removal of the bone outgrowth and the inflamed bursa can also be done with open surgery.
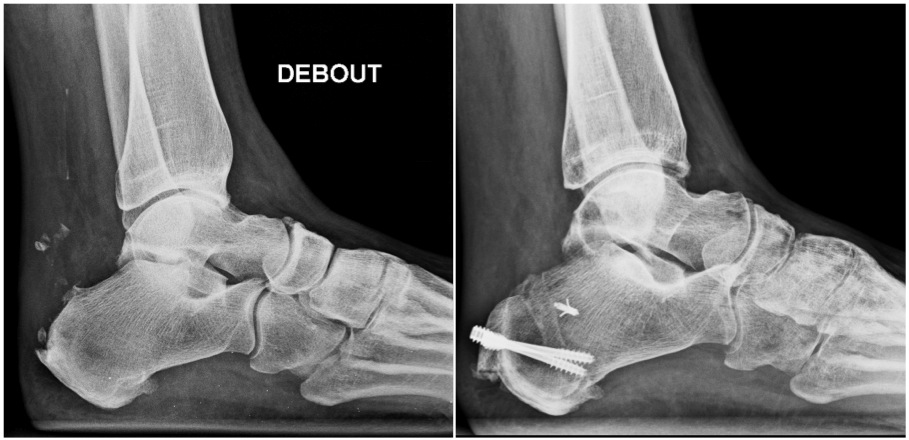
- Another technique is taking out a piece of bone from the heel bone through an osteotomy. However, this requires a longer rehabilitation, since the two bone fragments, fixed with a screw, will only fuse again after a 6 weeks minimum. During that period, the patient cannot lean on the ankle and often a plaster is needed.

